Surgical Removal of Mucocele and Ranula
Removal Of Mucoceles
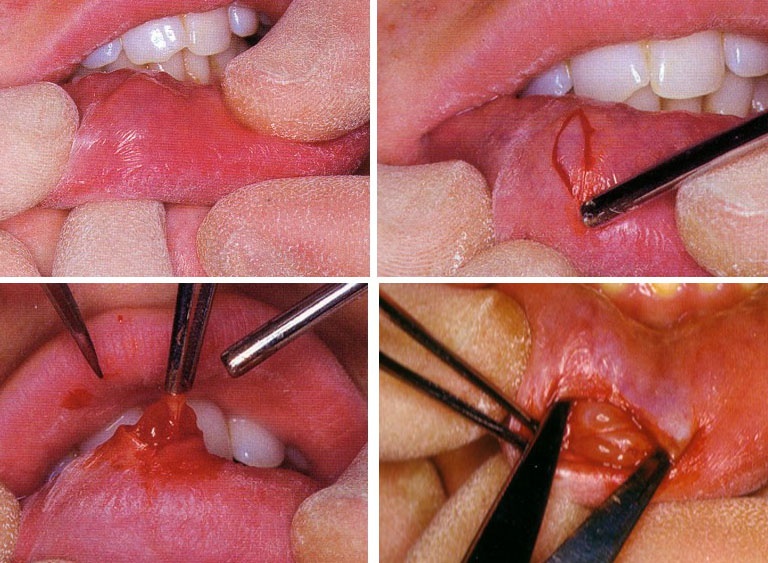
Surgical excision of the lesion is performed under submucosal ring block anaesthesia or, when the mucoele is in the lower lip, bilateral mental nerve block. (Fig. 1)
• Incision: For stabilization of the lesion a suture can be passed under it. Tension can be applied on the tissue throughout the procedure using this suture. A wedge shaped elliptical incision is then performed to include the lesion.
• Removal of the lesion: The tissues are then separated from the underlying submucosa using sharp dissection. Frequently minor salivary glands are encountered during the removal which should be removed. Surgical trauma may lead to development of mucoceles in these minor glands.
• Suture: The margins of the wound are undermined and the wound is sutured. Sutures should be performed through the mucosal layer only to avoid possible trauma to the minor salivcary glands in the area. Sutures are removed 5-7 days postoperatively.
Removal Of Ranula
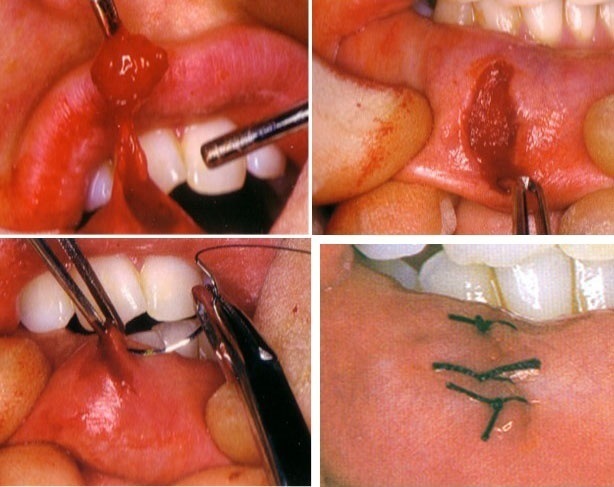
Surgical treatment of ranula can be done by either marsupialization or excision. However, excision of ranula is very difficult and is only indicated when the lesion is deeply located. Marsupialization is usually the treatment of choice. Excision of the superior wall of the lesion and suturing of the inner wall to the mucosa of the floor of the mouth is performed. This is accomplished by placing a series of interupted sutures arround the peiphery of the lesion, outlining its margins. The rof of the cyst is then exicised along the interior outline of the previously placed sutures. (Fig. 2)
Fig. 2: Diagram showing the surgical removal of Ranula. An incision is done on the roof of the ranula through the mucosa of the floor of the mouth and the wall of the lesion (upper left). After removal of the cystic fluid using suction the cystic cavity is filled with gauze until the cavity is completely outlined (upper right) A single suture is placed at the middle of the incision, the mucosa and the cyst lining are then cut from the top of the gauze filled cavity (lower left). Sutures are placed around the periphery of the lesion to join the cystic wall with the mucosa of the floor of mouth (lower right)
Transoral Sialolithotomy (Salivary Stone)
Transoral Sialolithotomy Of Submandibular Duct
• Anaesthesia: Surgical removal of salivary stone located in the submandibular gland duct is best performed under local anaesthesia with the patient in sitting position. Lingual nerve block is usually suitable for performing thisa procedure.
• Localization of the stone: The stone is located accurately by radiographs and palpation. A suture is passed through the floor of the mouth below the duct and behind the stone and tied. This suture will prevent the backward displacement of the stone along the duct which is especially possible if the stone is small and smooth.
• Retraction of the tongue: A suture is passed through the tip of the tongue. This suture is used to obtain retraction and control of the tongue during the surgical procedure.
• Incision: Care should be taken during performing the incision to avoid injury to the sublingual salivary gland and the lingual nerve. At the posterior part of the duct the lingual nerve lies lateral to it then crosses over the duct to pass medially and deep.
- If the stone in in the posterior part of the duct: The incision must be shallow and blunt dissection is imployed to prevent injury to the lingual nerve.
- If the stone is in the anterior part of the duct: The incision is designed to be over the stone and medial to the plica sublingualis to avoid injury to the sublingual gland.
• Dissection: Dissection is continued bluntly in the loose tissue until the duct is encountered, if the lingual nerve is encountered it should be retracted carefully. Bleeding is usually not a problem but if occured it should be controlled by ligation to ensure adequate visulization during stone removal. The duct is best identified at the site wher the stone is lodged, if not possible, a probe may be passed into the duct to aid its visualization.
• Incision of the duct: Once identified at the site where the stone is lodged the duct should be incisied longitudinally over the stone. Never cut the duct transversely as retraction of the two parts of the duct may complete the cut and a salivary fistula may result.
• Removal of the stone: The stone can usually be removed with small forceps. However, large stellate stones may need to be crushed before removal. After stone removal a small aspirating canula is passed toward the duct to aspirate any pus, mucous plugs, small pieces of crushed stones that may remain. A probe is then passed from the orifice to the surgical opening to ensure patency of the anterior part of the duct.
• Closure: The wound edges are sutured at the level of the mucosa only. No effort should be made to clsoe the duct as recanalization will occur. (Figs 7-3 and 7-4)
Transoral Sialolithotomy Of Parotid Duct
• Incision: Local field block anaesthesia or general anaesthesia may be used. Generally removal of a stone in the parotid duct is much more difficult than removing it from the submandibular gland. A direct cut down on the stone, as the case with submandibular duct stone, is only possible when the stone is located infront of the anterior border of the masseter. Stones located further backwards are approached through a semilunar incision runung from above downwards inftront of the duct orifice. (Fig. 7-5)
• Dissection: Dissection is carried out bluntly to expose the duct. The mucosal flap and the duct are then retracted medially while the check is retracted laterally. Access to the more posterior segment of the duct is done by following the duct paoteriorly by blunt dissection.
• Removal of the stone: When the stone becomes accessible, a longitudinal incision is made through the duct over the stone on the lateral aspect of the duct and the stone is removed.
• Closure of the wound: Suturing is performed on the mucosa only and no attempt is made to sutur the duct. Recanalization will occur.
Surgical Excision Of Sublingual Gland
Surgical Excision Of Submandibular Gland
Incision
An extraoral submandibular incision is used. The incision should follow the course of the diagastric muscle. To determine the course of the diagastric an imaginary curved line is drawn to connect the mastoid process, the lateral surface of the hyoid bone and the genial tubercle. A 5 cm long incision is made along the middle segment of this curved line. The incision well be directly over the inferior pole of the gland. The incision is made through the skin, superficial fascia and platysma muscle. (Fig. 7-6)
Dissection
• Skin and superficial fascia are reflected inferiorly exposing the anterior facial vein crossing the submandibular gland. The vein is isolated, ligated and cut between the ligations.
• The upper flap is raised close to the surface of the gland using scissors. The plane of dissection should pass deep to the remnants of the anterior facial vein to ensure that all branches of the facial nerve will be raised with the flap. The cervical branch of the facial nerve is usually encountered at this level and can usually can be retracted. However, cutting this branch presents no serious loss of function as it supplies, only partially the platysma muscle.
• By blunt disection the gland is freed anteriorly and inferiorly. The gland is then retracted upward and backward. The posterior belly of diagastric and the stylohyoid muscle anterior to it are identified. The muscles are retracted downward to expose the facial artery as it lies between the gland and the muscles. The facial artery is clamped and ligated.
• The upper flap, with the anterior facial vein, is retracted and the interval between the gland and the inferior border of the mandible is defined. At the sametime, the gland is reflected up and backward exposing the posterior border of the mylohyoid muscle. Using finger dissection the gland is further freed. Care should be taken to protect the hypoglossal nerve which lies medial to the gland as it crosses over the underlying hupoglossus muscle.
• The gland is then retracted downword and detached from its attachments with the submandibular ganglion. The lingual nerve can be idenbtified at this point and avoided.
• The mylohyoid muscle is retracted anteriorly and the submandibular duct retracted posteriorly. The duct is ligated by two sutures anterior to the ductal pathosis, if exist, and cut between the ligations. This is to prevent the sepage of infected material into the wound from either the residual duct or the gland. The gland is then removed.
Closure
The resulted dead space must be closed or drained. Drainage is indicated whenever there is doupt that the field is infected. Wound clousre is performed as follows:
• The fascia of the diagastric, mylohyoid, hyoglossus and stylohyoid muscles are approximated and sutured using absorbable catgut.
• The subcutaneous tissues are sutered using resorbaple catgut.
• Skin is sutured using 4-0 black silk and the sutures are removed 5-7 days postoperatively.
Postoperative Care
• The wound should alawys be covered with heavy pressure dressing. This will help to eleminate any dead space and help drainage.
• The draine should emerge from the most dependent point, which is usually the posterior aspect of the wound. The draine is removed 24-48 hours postoperatively, if no wound suppuration is present.
• Five days postoperatively the dressing may be discontinoued and half the sutures are removed. Adhesive tabe should pridge the incision line.
• The remmining sutures are removed 7 days postoperatively but the wound should continue to have adhesive tabe bridging support for at least two weeks.
Surgical Excision Of Parotid Gland
Because of the possibility of permenant damage to the facial nerve and its branches removal of the parotid gland is only performed when stronge indications are present and after faliure of all conservative methods of treatment. The presence of tumors or suspected malignancy are the primary reasons for removal of the parotid gland. (Fig. 7-7)
Incision
Incision for removal of the parotid gland runs from the superior attachment of the auricle downwards, turns anteriorly at the angle of the mandible to the submandibular region to stop at the hyoid bone. A second incision is made posterior to the pinna and join the first one anterior to it. By blunt dissection the ear is retracted from the field and a skin flap is developed over the cheek side of the incision. (Fig. 7-8)
Localization of the facial nerve
The facial nerve can be located by one of the two following ways:
• Locate the peripheral portion of the branches of the facial nerve as they emege from the anterior border of the gland and dissect backwards.
• Locate the main trunk of the facial nerve by dissecting between the posterior border of the gland and the stylomastoid foramen and dissected anteriorly. A nerve stimulator is very helpful during localization of the facial nerve and its branches.
Dissection and wound closure
• The superficial lobe (Suprafacial part) of the gland is then dissected out and removed. The duct is ligated and cut in the same way as the submandibular duct.
• Disection of the deep lobe is facilitatated by posterior and superior retraction of the ear. Care should be taken to protect the external carotid artery and the retromandibular vein which pass through the gland..
• The wound is then closed in layers and a draine is inserted to be removed ater 48 hours.
Complications Of Salivary Glands Surgery
Ductal Stricture
Stricture of the duct may occur following biopsy or other surgical procedures near the duct or its orifice or following transeverse incision of the duct.
Treatment
• Mild stricture as those resulting from inflammation are treated by mechanical dilatation of the duct and/or with administration of sialogague.
• Stricture close to the orifice are treated by papillectomy.
• Stricture along the ductal course is treated by surgical repositioning of the ductal opening. The duct is isolated and sectioned proximal to the stricture. The distal end of the proximal portion is then repositioned to a new surgically created opening. (See Fig. 6- )
• Stricture close to the gland may need gland removal.
Salivary Fistula
Salivary fistula may result from ulceration of the duct by a stone, surgery on the duct or the gland or may be congenital. Intraoral fistulae are usually symptomless while extraoral fistulae are troublesome and may be accompanied by swelling. Treatment of extraoral fistulae is usually surgical repaire or glandular excision.
Facial Nerve Paralysis
Facial nerve paresis or paralysis may occur following surgery on the parotid gland. Temporary paresis is due to decrease conductivity of the nerve secondary to repeated stimulation during the operation and postoperative edema.