Disorders Of Salivary Glands
The salivary glands disorders are classified into developmental, functional, obstructive, inflammatory, neoplastic and allied conditions (Table 1). Developmental anomalies of the salivary glands include aplasia, atresia and aberrancy. Aplasia is congenital absence of salivary glands and its quite rare. Atresia, on the other hand, is congenital absence or occlusion of the ducts and it is also very rare. Aberrancy is abnormally placed salivary tissues.
Table 1. Classifications of salivary glands disorders.
Developmental Disorders
- Aplasia.
- Atresia.
- Aberrancy.
Functional Disorders
- Sialorrhea.
- Xerostomia.
Obstructive Disorders
- Sialolithiasis.
- Strictures.
- Mucocele.
- Ranula.
Inflammatory Disorders
- Acute sialoadenitis.
- Chronic sialoadenitis.
- Mumps.
- Postirradiation sialoadenitis.
- Postsurgical sialoadenitis.
- Salivary glands inclusion disease.
- Necrotizing sialometaplasia.
Neoplastic Disorders
A. Benign neoplasms
- Pleomorphic adenoma.
- Adenolymphoma.
- Oncocytoma
B. Malignant neoplasms
- Malignant pleomorphic adenoma.
- Adenmococystic carcinoma.
- Mucoepidermoid carcinoma.
- Acinic cell carcinoma.
Allied conditions
- Sjogren's syndrome.
- Mikulicze's syndrome.
- Sarcoidosis.
- Sialoadenosis.
Functional Disorders
Sialorrhea (Ptyalism)
Sialorrhea is excessive salivary flow. The condition may result from many causes that may be categorized into two groups:
- Conditions affecting the central nervous system: This includes mental retardation, epilepsy, and other mental and psychological disturbances.
- Local factors that reflex stimulate salivary flow: The most common cause in this category is acute oral inflammation as herpetic stomatitis, Vincent's infection and aphthus ulcers. Other causes include teething and ill-fitting dentures. Usually treatment of the infection and/or removal of the cause affect cure.
Xerostomia
Xerostomia or dryness of the mouth results from diminished salivary secretion. Xerostomia is diagnosed when the salivary flow is equal to or less than 2 ml / 15 min which is less than 4% of the normal flow.
Xerostomia may be idiopathic or due to local and systemic causes. Local causes include mouth breathing, salivary gland inflammation, irradiation and aging changes. Systemic causes, on the other hand, include anemia, emotional and anxiety status and fluid loss. Clinical findings of xerostomia are listed in table 2.
Treatment of secondary cases of xerostomia is usually the removal of the underlying factors while treatment of idiopathic cases is usually symptomatic. Mouth wash containing citric acid, lemon essence and glycerin is prescribed to the patient in addition to good dental home care and frequent dental treatment visits. This is very important to prevent dental and oral complications which may develop.
Table 2. Signs and symptoms of xerostomia.
- Dryness of the mouth.
- Tongue redness with papillary atrophy and fissuring.
- Taste disturbances.
- Denture wearing difficulties.
- Increase carious index.
Obstructive Disorders
Mucocele
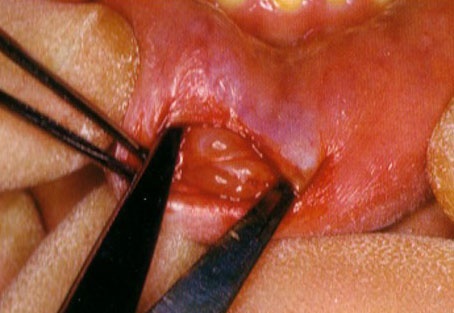
Mucocele is a fluid or semifluid filled cavity that is surrounded either by compressed granulation tissues of epithelium. The lesion is due to obstruction of the salivary duct which result in accumulation oft he salivary flow and dilatation of the duct wall. This type is referred to as a retention cyst and it may be considered as a true cyst as it is lined by epithelium tissue. Extravasation mucocele, on the other hand, is not a true cyst. It is due to rupture of the duct with escape of the salivary flow into the surrounding connective tissue. The resultant mucous pool is lined by compressed granulation tissue. (Fig 1)
Blandin-Nuhan cyst is a mucocele that involves the minor salivary glands on the under surface of the anterior part of the tongue, while Ranula is a mucocele which occur on the anterior part of the floor of the mouth.
Although mucocele may occur at any where in the oral cavity, yet the most common site is the lower lip. The lesion varies in size from few millimeters to centimeter or more and may be superficially or deeply located. When superficially located it may have bluish translucent color. The common occurrence of the lesion on the lower lip was attributed, by some authors, to the habit of lip biting which usually involve the lower lip leading to either obstruction of the duct of the minor glands or its rupture. Treatment of the conditions is by surgical excision of the lesion with the surrounding salivary tissues.
Ranula
Ranula is a mucocele which occur on the anterior part of the floor of the mouth (Fig 2). The lesion is usually superficial and unilateral with average size of 2-3 cm. On palpation the lesion is soft and fluctuant and has a bluish-violet color.
The walls of the ranula are very thin and composed of either epithelium of compressed granulation tissue and it contains a viscous mucoperiosteum fluid. Successful treatment is surgical marsupialization of the lesion.
Sialolithiasis (Salivary stones)
Sialolithiasis is the formation of calcific concretions within the ductal system of the salivary glands. It is one of the most common disorders of the salivary glands. It occurs in males twice as frequently as in females with the peak of age incidence between 30-50 years. The submandibular gland is the most common site for salivary stones (80%) followed by parotid gland (19%) while it is quite uncommon to occur in the sublingual or the minor glands. (Fig 3)
The exact etiology of the salivary stones is unknown. However, three prerequisites are suggested to be the primary etiological factors. These are:
- A neurohumoral condition that result in salivary stagnation.
- A nidus or a matrix for stone formation.
- A metabolic mechanism favoring precipitation of salivary salts into the matrix in the presence of a coexisting inflammation. This factor is affected by the pH of the saliva. This explain why salivary stones are much more common in the submandibular gland which is more alkaline than the parotid gland.
Signs and symptoms of salivary stones vary. However, intraglandular stones generally cause less sever symptoms than the extraglandular intraductal stones. Sialolithiasis can be presented clinically in one of three basic forms. These are symptom-free, transient swelling and acute suppurative inflammation (Table 6-3). Diagnosis of salivary stone is usually done by palpation and radiographic examination. Palpation along the course of the duct will confirm the presence of a hard stone.
Stensen's duct stones: May occur either in the intraglandular part, the extraglandular part lateral to the buccinator muscle, the submucosal part or may be found impacted at the papilla. Usually the stone can be seen on radiographic examination and palpated except if in the intraglandular part of the duct.
Whartone's duct stones: Salivary stones is the most common disorder of the submandibular gland. The most common location of the stone is the extraglandular part of the duct. Stones in Whartone's duct may reach quite large size and yet remain painless and symptom-free. This is attributed to the larger lumen and the more expendability of the duct.
Treatment
Treatment of salivary stone is essentially surgical by removing the calculi. However, surgery is not allowed during the inflammatory phase. Antibiotics, analgesics and antipyritics are given to the patient until subsidence of the acute phase before surgery is performed.
Table 3. Signs and symptoms of salivary stones.
Symptom-free Cases
- Occasionally there may be total absence of subjective symptoms.
- This cases are usually discovered accidently during radiographic examination for other problem.
- The stone partially obstruct the canal.
Intermittent Transient Swelling Of The Gland
- Eating initiates intermittent transient swelling of the involved gland.
- The swelling subside between meals as the stone is not occluding the duct completely so when the salivary demands diminished the saliva escape from around the stone and the swelling subside.
- There is moderate discomfort of the patient.
Acute Suppuration
- Pus is seen exudating from the duct orifice.
- Soft tissues surrounding the duct shows sever inflammatory reaction, i.e. redness, hotness, swelling and tenderness.
- The gland is enlarged tender and tense.
- Pain on palpation of the gland and the duct.
- Episodes of pain whenever the gland increases its production of saliva as at meal time.
- Spontaneous exfoliation of the stone may occur.
Ductal Stricture
Ductal stricture usually result from resolution of ulceration of ductal lining which occur due to the presence of a salivary stone. Also horizontal incision of the duct, during surgical removal of a stone, may result in stricture while longitudinal incision do not. Stricture near the papilla is treated by papillotomy while those situated more posterior are treated by sialodochoplasty. On the other hand, stricture close to the gland will require removal of the entire gland.
Treatment
- Dilatation: Stricture of parotid duct can be managed by dilatation using a suitable size probes that pass one after another through the duct. The procedure may need to be repeated 2-3 times at two weeks interval. Dilatation may remain effective for considerably long time.
- Papillotomy: When the stricture is close to the papilla, the portion of the duct anterior to the stricture is laid opened using a fine scissor after insertion of a fine probe to serve as a guide for the duct. Starting from the papilla the cut is carried posteriorly until the dilated area proximal to the stricture is reached. The duct lining is then sutured to the mucosa of the floor of the mouth using 5-0 chromic suture.
- Sialodochoplasty: This means implantation of the submandibular duct into the floor of the mouth. The duct must be divided and implanted into a new position. It is used when papillotomy is not successful and the opening is closed after short time.
Inflammatory Disorders
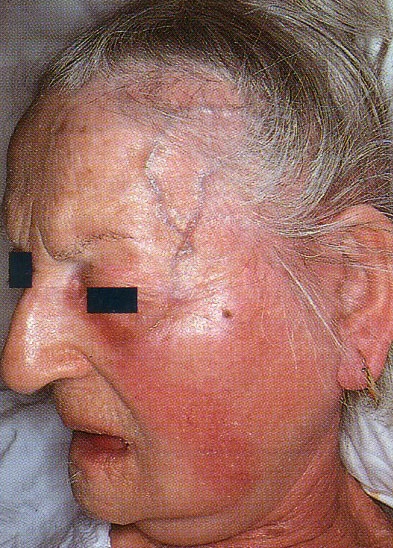
Acute suppurative parotitis in an old female patient
Note hot, red and board-like swelling with distended temporal veins
Acute Sialoadenitis
Sialoadenitis means inflammation of the salivary glands. It occurs much more common on the parotid gland than in the submandibular gland. Non specific forms of sialoadenitis occurs due to mixed infection that ascend to the gland via the duct, while specific forms (e.g. Mumps) are mostly blood-borne. Diagnosis is usually not a problem basing on the clinical picture and laboratory findings (Table 6-4). Generally the condition is a disease of elderly, dehydrated, malnourished patient, as well as, chronically ill patients. Table 6-5 shows a list for the treatment modalities for acute sialoadenitis. However, once sialoadenitis has occurred it tends to reoccur frequently in the subacute or chronic forms. This is especially true in elderly and compromised patients.
Chronic Sialoadenitis
Chronic sialoadenitis is similar to that of acute form of the disease but symptoms are less sever. Usually there is no erythema and tenderness of the skin overlying the gland.
In the submandibular gland the condition is almost exclusively a complication of ductal obstruction which cause ductal dilatation and salivary stasis. This is followed by glandular atrophy and fibrosis. Retrograde invasion of bacteria via the duct result in abscesses formations. In the parotid gland, on the other hand, the route of infection is less understood. However, low secretion rate of parotid may be a predisposing factor.
Diagnosis is based on the presence of paste history of acute sialoadenitis or glandular pain and/or swelling. Sialogram may show "Pruned tree" appearance due to lack of aciner filling. Long standing cases show "Punctate-dilatation" appearance of the peripheral ductules. Treatment of the chronic sialoadenitis is listed in table 6.
Chronic recurrent parotitis in children
This condition occurs mostly in children at the age of 3-6 years. It is characterized by its unilateral occurrence and spontaneous healing. Sialograms show normal ductal architecture. Treatment is symptomatic. The condition must be differentiated from mumps. Differentiation can be done by the following criteria:
- The condition occurs unilaterally while mumps is always bilaterally.
- Purulent material could be expressed from the gland in chronic recurrent parotitis.
- In mumps virus can be detected in the saliva by complement fixation test.
Sialectasia
The symptoms of this condition is similar to those of chronic recurrent sialoadenitis. However, there is some disagreement about the nature of the disease. It has been stated that the condition is not a disease but rather a sign for an inflammatory reaction in the gland.
Mumps (Epidemic Parotitis)
Mumps is a nonsuppurative, acute sialoadenitis of viral origin. It is a highly infectious disease that is presented clinically as a painful enlargement of one or more of the salivary glands. It usually affects children between 6-8 years of age. The most common affected salivary gland is the parotid and in 10% of cases the submandibular gland become affected as well. The virus may affect other organs as pancreas, testis and ovaries. Clinical signs and symptoms of viral mumps are listed in table 6-7 and its complications are listed in table 8.
Mumps usually resolves spontaneously within 5-10 days. Accordingly, treatment include symptomatic relief of pain and fever and prevention of dehydration. Persistent or recurrent cases are indicative for development of chronic bacterial sialoadenitis secondary to viral mumps.
Post Irradiation Sialoadenitis
Patient receiving radiation for malignancies in the head and neck usually develop an acute inflammatory reaction within the salivary glands. There may be xerostomia, and swelling of the parotid and submandibular gland which increase for 12-24 hours then rapidly subside without treatment. Over the period of the irradiation therapy degenerative changes occur that may lead to atrophy of the gland.
Post Surgical Parotitis
This condition develop 4-6 days after surgery and the symptoms are very similar to those of acute sialoadenitis. Predisposing factor is diminished salivary flow after surgery which is probably due to dehydration and fever and trauma to the gland by prolonged pressure from an anesthetic mask. Treatment include fluid intake, stimulation of salivary flow, antibiotics and analgesics.
Salivary Gland Inclusion Disease
The condition also called "Cytomegalic Inclusion Disease" and it results from infection by cytomegalovirus. The majority of cases occur in infants below 2 years of age. The disease may be acquired inutero or at any time postnatally. The organs most often affected are salivary glands, kidneys, pancreas, liver, lungs and thyroid gland.
Cellular changes which occur in the affected gland include the appearance of large intranuclear bodies with less distinct cytoplasmic inclusion bodies. The parotid gland is most often affected in infants and children while the submandibular gland is more frequently involved in adult cases.
Most cases of inclusion disease in the salivary glands are subclinical. However, in newborn and infants a serious disease may result that is characterized by prematurity, intracranial calcifications and hepatosplenomegaly. Diagnosis depends on the identification of the virus in the saliva, urine, blood or tissues of the patient.
Necrotizing Sialometaplasia
This condition affects mostly the minor salivary glands of the hard palate. It occurs more commonly in men than women. Clinically the lesion may be mistaken for mucoepidermoid carcinoma or squamous cell carcinoma. The lesion appears clinically as ulceration on the mucous membrane that vary in size from 1-3 cm. Swelling and a feeling of fullness may precede the appearance of some lesions. Pain is not a common symptom. (Fig 5)
The most likely etiology of the disease is local ischemia of the minor salivary gland that result in squamous metaplasia of the ductal epithelium. The cause of this local ischemia is unknown. The use of alcohol, tobacco and drugs, as well as diabetes and wearing ill fitted dentures have all been suggested as a predisposing factors.
The condition is self-limiting and heals by secondary intention over a period of 6-8 weeks. Lesion debridement and the use of saline mouth wash may aid in the healing process. Recurrence is quite uncommon.
Neoplastic Disorders
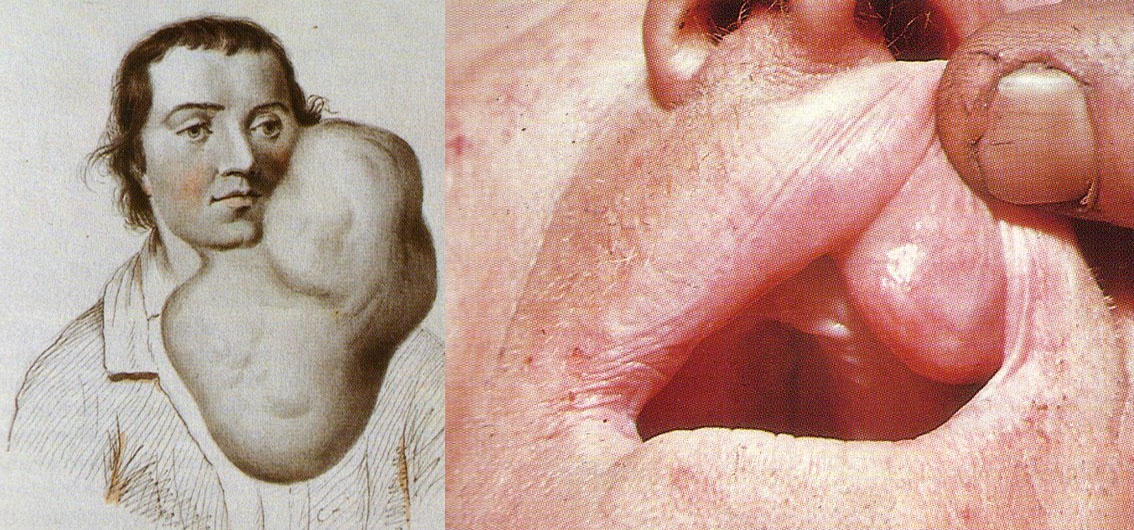
Pleomorphic adenoma is a slowly growing benign salivary glands tumor that may attain a very huge size. On the left side is a drawing from the eighteenth century for a very huge case of benign pleomorphic adenoma of the parotid gland.
To the right is a pleomorphic adenoma on the upper lip.
Benign Neoplasms
Benign pleomorphic Adenoma (Benign Mixed Tumor)
Benign pleomorphic adenoma is the most common neoplasm of all salivary glands tumors. It comprises 90% of benign tumors and 50% of all tumors affecting salivary glands. Clinical features of the tumor are shown in table 9. (Fig 6)
Histologically there are diverse histological pattern. Cuboidal, stellate, polyhedral, spindle or squamous cell element may be found in the connective tissue stroma. The stroma in itself show a variety of mucoid, myxoid, chondroid or hyaline pattern. However, ossification foci rarely occur.
Treatment and prognosis
The tumor is radioresistant and the only treatment is surgical removal. Surgical removal of the whole gland is usually necessary in cases of submandibular and sublingual glands. For parotid tumors, on the other hand, the surgical excision ranges from removal of the entire involved lobe to careful local excision. This is due to the presence of important vital structures that pass through the substance of the parotid. These are the facial nerve and the external carotid artery and the retromandibular vein. Minor salivary glands lesions are treated by removal of the tumor mass with margin of surrounding normal tissues. Prognosis is very good and recurrence is not more than 1% and usually due to incomplete removal.
Adenolymphoma (Warthin's Tumor) (Cystadenoma Lymphomatosum)
This tumor is the most common of all monomorphic salivary glands tumors. Characteristically adenolymphoma is the only salivary gland tumor that:
- Frequently found bilaterally, which point to a possible multifocal origin (30% of cases).
- Occurs more in males over the middle age.
The most common site for this tumor is the lower lobe of the parotid gland, but it has been reported in all other major and minor salivary glands. It appears as a slowly growing painless firm swelling that is superficially located and rarely exceeds 3-4 cm in size (Fig 8). Treatment is surgical excision and recurrence is rare.
Histologically the tumor composed of two components, epithelium and lymphoid. Accordingly, it has been suggest that the tumor originates from inclusion of salivary duct epithelium with the substance of a lymph node which, in turn, becomes entrapped in the late encapsulated parotid gland. Lymphoid element may be only a passive element.
Oxyphilic Adenoma (Oncocytoma)
This tumor is a rare slowly growing tumor that is usually small in size. The most common site is the parotid gland, but other glands may be affected. It affects females more common than males usually over the seventh decade of age. Clinically it appears as firm, freely mobile small encapsulated mass. Histologically it consists of cells closely resembling oncocytes (a normal cell found in the ducts of old persons). Treatment of surgical excision of the tumor and it has no tendency to reoccur.
Malignant Neoplasms
Malignant Pleomorphic Adenoma
There is some doubt whether this tumor represent a malignant transformation in a benign pleomorphic adenoma or it is a malignant tumor from the start. The clinical difference between the benign and malignant form is the presence of pain, fixation and ulceration. Lymph node involvement and distant metastasis may occur. Treatment is surgical excision and recurrence is quite frequent.
Acinic Cell Carcinoma
This is a moderately malignant tumor that is almost entirely limited to the parotid gland, usually in persons over the middle age. Clinically the tumor appears as a small, round encapsulated firm mass which may be fixed to the surrounding tissues.. Pain is not a feature. Histologically it is composed of cells resembling normal serous aciner cells hence the name "acinic cell carcinoma". Treatment is surgical excision with safety margin and recurrence occur in 50% of cases.
Adenoid Cystic Carcinoma
Adenoid cystic carcinoma is the commonest minor salivary glands tumors. The palate is the most common site. Females are more commonly affected than males usually over 50 years of age. When it occurs in the major salivary glands the tumor do not show any sex predilection. Clinically the tumor is represented as a firm mass that is fixed to the surrounding tissues. Ulceration of the overlying mucosa is common. Pain and paresthesia are frequently associated with the tumor. This was attributed to the tendency of the tumor for perineural or intraneural invasion. (Fig 9)
Histologically the tumor composed of small cells arranged in "Swiss-cheese or Clyindromatous pattern". Occasionally, it may have a "Solid Pattern" that makes the diagnosis more difficult.
Treatment has been suggested to be the most radical surgical procedures together with radiotherapy. The tumor has a recurrence tendency and gives early metastasis. Clinical experience has suggested that there is a correlation between the site and the prognosis of the tumor. Tumors in the minor salivary glands of the palate has the best prognosis and those of the submandibular gland has the poorest prognosis.
Mucoepidermoid Carcinoma
This is the most common malignant tumor of the major salivary glands. Of the major salivary glands the parotid is the most commonly affected while the palatal glands are the most commonly affected of the minor salivary glands (Fig 10). It usually occurs between 4th and 6th decade of life and has no sex predilection. Clinically and histologically mucoepidermoid carcinoma has two types:
- Low-grade tumor: Appears as a soft, slowly growing painless mass, usually small in size (5 cm). The mass may be cystic and containing mucoid material. Histologically it is composed of mucous and epidermoid cells arranged in duct-like pattern.
- High-grade tumor: Appears as a firm less cystic rapidly growing mass. Pain is more frequently an early symptom. Histologically it is composed of epidermoid and intermediate cells. Cysts and ductal elements are absent. Both forms are not encapsulated.
Treatment of the tumor is surgical excision. Local excision has been proved to be adequate for low-grade tumors, provided that it has been completely removed. Despite the more radical surgical excision used for removal of low-grade tumors recurrence is much more common. Those of the minor salivary glands still have poorer prognosis.
Allied Conditions
Sjogreon's Syndrome
This is a disease that consists of chronic inflammation of the lacrimal and salivary glands, keratoconjunctivitis sicca, xerostomia and rheumatoid arthritis which occurs in 50-60% of cases. The condition often affects females over 50 years of age. When the condition is not associated with rheumatoid arthritis it is called "Sicca syndrome". In some cases there is enlargement of the salivary glands usually the parotid bilaterally.
The disease is suggested to have an autoimmune nature. A genetic predisposition has also been suggested. Microscopically there is focal lymphatic sialoadenitis of the major as well as the minor salivary glands. Accordingly, minor glands biopsy is diagnostic. Patients suffering form this condition has a strong tendency for development of extrasalivary lymphatic abnormalities, e.g. malignant lymphomas.
Treatment of this condition is a challenge and is usually symptomatic. Clinical evidences suggests improvement after removal the affected salivary glands. This results, most probably from improvement of the immunological status of the patient.
Lymphoepithelial Lesion (Mikulicz's Disease)
It is asymptomatic enlargement of the salivary and lacrimal glands. It has been suggested that the condition is closely related to Sjogreon's Syndrome and that both are autoimmune diseases. Surgical treatment and radiotherapy has both been used in the treatment with successful results. Malignant behavior with development of lymphomas and carcinomas within the benign lymphepithelial lesion has been reported.
Sarcoidosis
Sarcoidosis is a chronic granulomatous disease of an unknown origin affects mostly young and middle age persons. It is characterized by enlargement of the lymph nodes in different parts of the body and the formation of small granulomas in the lungs, liver and spleen. Clinical manifestation of sarcoidosis are listed in table 10. No specific treatment for sarcoidosis is known.
Sialoadenosis
Sialoadenosis is a nonspecific term used to describe a noninflammatory, nonneoplastic enlargement of the salivary glands, usually the parotid. There are four forms of sialoadenosis which are metabolic, nutritional, alcoholic and drug induced gland enlargement.
- Metabolic or endocrine sialadenosis: Some metabolic disorders has been proved to be associated with asymptomatic parotid gland enlargement.
- Nutritional sialadenosis: All conditions of starvation or malnutrition predispose to parotid enlargement. The term "Nutritional mumps" has been applied to this condition.
- Alcoholic sialadenosis: The association of sialadenosis and alcoholic cirrhosis of the liver is now well documented. The parotid gland swelling may focus attention to the underlying liver condition. Improvement of the parotid swelling seems to be associated with the improvement of the liver condition.
- Drug induced sialadenosis: An inflammatory swelling of the salivary glands may occur after injection of certain heavy metals. The glands are enlarged edematous and tender. "Iodine mumps" which is a diffuse tender swelling of the salivary glands and the surrounding tissues sometime develop after injection of iodine containing compounds. The swelling subsides within 4-6 days. The submandibular gland is more commonly affected.