MANAGEMENT OF PATIENTS RECEIVING LOCAL ANALGESIA
Patients who are going to receive local anaesthesia should be managed properly to obtain good anaesthesia without complication. To achieve this goal preanesthetic evaluation of the patient is essential together with proper preparation for injection and injection technique.
PREANALGESIC EVALUATION
A. Case History
Taking through case history is very essential. This should include personal history, history of chief complaint, history of present illness, past dental and medical history, familial history as well as review of systems. Importance of case history are listed in table 6-1.
Never forget to ask the patient if he had a similar procedure done to him before and if he had any complications or difficulties during or after anaesthesia.
B. Local Examination
Careful examination of the region of operation should be performed to evaluate the time required to perform the surgery and its severity. Observe the normality of the anatomical structure in the area and detect any obstacles in the site of injection whether mechanical or septic.
C. Inform The Patient About The Procedure
The dentist should explain to the patient in a simplified way the nature of the treatment he is going to receive. This is important to gain confidence of the patient and to allay his apprehension. Never lie to a patient, especially children, otherwise "dental fear complex" will develop.
Patients Groups
According to the data obtained from case history and clinical examination, patients can be divided into three groups regarding their suitability to receive local anaesthesia.
• Group I: Include those patient to whom the use of local anaesthesia is strictly contraindicated and has to be given general anaesthesia.
• Group II: Include those patients that have to be carefully examined and evaluated before giving local anaesthesia. Cosultation with specialists and physicians is a must.
• Group III: Include those patients who are fit to receive local anaesthesia. They are subdivided into two subgroups:
- Subgroup 1: Includes those patients who are ready to receive local anaesthesia without any premedication.
- Subgroup 2: Include those patients who require premedication such as sensitivity test and tranquilizers.
Sensitivity Tests
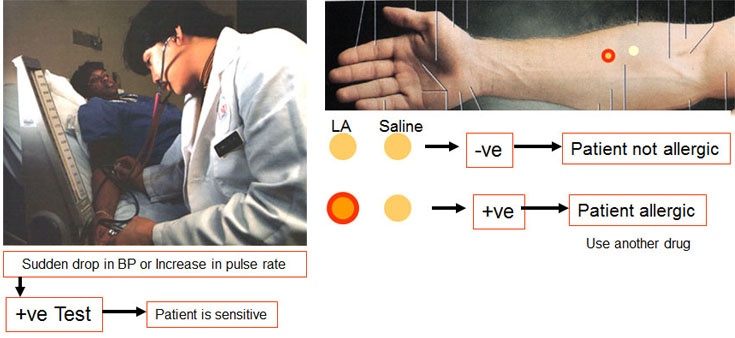
A. Skin Test
The test is done by injecting a small amount of the anesthetic drug in the forearm and inspecting the reaction after 5 minutes. Technique is as follows:
- Clean the anterior surface of the forearm and sterilize it using alcohol or any other suitable disinfectant solution.
- A small intradermal wheal, about 1/2 cm in diameter, is raised by injecting saline solution using a suitable needle and syringe.
- A similar wheal is raised, 3-4 cm away from the saline wheal, by injecting the local anaesthetic solution.
- After about 5 minutes examine the two wheals, if they are similar, the test is negative and the patient is not allergic to the anesthetic solution used. If the second wheal becomes red in color and spread over a wider area, the test is positive and the patient is sensitive to the anaesthetic solution used.
B. Intranasal Test
This test is performing by applying the anesthetic solution to the nasal mucosa while the blood pressure and the pulse of the patient is being monitored for any changes. This test should always supplement the skin test. The test is performed as follows:
- The patient is placed in supine position with the sphyngno-manometer cuff applied to one arm.
- Blood pressure and pulse rate are recorded every 3 minutes until stabilized.
- One drop of the local anaesthetic solution is introduced in each nostril, then after 3 minutes two other drops are introduced. Note the blood pressured and pulse rate.
- After 3 more minutes 43 drops are introduced in each nostril and also record the blood pressure and pulse rate.
- The test is positive and the patient is sensitive to the anaesthetic solution if sudden drop in the blood pressure and increased in the pulse rate occur.
Never do sensitivity test to disprove allergic history. The amount of the anaesthetic drug used in the test, although very small, yet it may precipitate a sever allergic reaction that may be quite harmful to the patient.
PREPARATION FOR INJECTION
The site of injection and the patients mouth should be prepared before injecting the anesthetic solution. The following are some important points:
- Suitable type of syringe and needle should be used, short needles for infiltration and long needles for nerve block technique. The syringe and the needle should be sterilized.
- The anaesthetic carpule should be sterilized from outside by placing it in a colored antiseptic solution, Then warmed to body temperature by holding it in hand. The solution should be colored so that if any leakage occurred and the anaesthetic solution becomes contaminated the color of the solution in the carpule will be changed. Also never use alcohol to disinfect the anaesthetic carpule as any possible contamination to the anaesthetic solution may lead to prolonged anaesthesia or even nerve damage.
- The operator should wear gloves when doing the injection.
- The patient mouth is prepared by doing scaling if needed and asking the patient to rinse with an antiseptic mouth wash.
- The site of injection is carefully cleaned from food debris and then sterilized by wiping it with disinfectant solution as 5% tincture iodine.
INSERTION OF THE NEEDLE
The key stone for performing successful injection is the proper insertion of the needle. The syringe is held in pen grasp position and the following points are to be remembered when inserting the needle:
- The site of needle insertion should be stretched to facilitate needle insertion.
- The bevel of the needle should be directed toward the bone and, in case of infiltration anaesthesia, the needle should be 45o angle with the cortical plate of bone.
- The prick should be made as quick as possible.
- The patient should be aware that he is going to have injection but not exactly when. The nervous system of the human being hats surprises and the reaction to a sudden painful stimulus, such as this of a needle puncture, may be unexpected from the patient, e.g. pushing the hand of the operator or sudden head jerky movement. This may result in needle breakage or otherwise harm to the patient.
- The needle should be bent inside the tissue, if you want to change the direction remove the needle and reinsert in the new desired direction.
- After insertion aspiration should be done to be sure that the needle is not in a blood vessel. Also the rate of injection should not exceed 2 cc/min.
- Aspirate and inject slowly:
- This is a golden rule that should be remembered for successful uncomplicated
administration of local anaesthesia. The administration of local anesthesia in dentistry is considered essential whenever potentially painful procedure is to be performed. However, it should be always remembered that local anesthesia, like any other drug,
has two types of reaction beneficial and harmful reaction. Overdose reaction, allergy and idiosyncrasy are some of the most important adverse reactions. Overdose reaction is refers to symptoms manifested as a result of absolute or relative over administration
of the drug which produces elevated level of the agent in the blood. Drug level in blood may be elevated as a result of administration of two large dose, rapid absorption of the drug into the circulation, intravascular injection or slow biotransformation and
elimination of the drug as in cases of renal and liver diseases. However, the most common cause for local anesthetic overdose is accidental intravascular injection. In addition rapid injection is painful and help the rapid absorption of the drug into circulation.
INJECTION TECHNIQUES
INFILTRATION TECHNIQUES
I. Submucosal Infiltration Analgesia
This technique is suitable for removal of hypertrophied soft tissues and high muscle attachments as well as similar procedures in patients of all age groups. The analgesic solution is deposited just beneath the mucosa.
II. Paraperiosteal Infiltration Analgesia
The success of this technique depends on the diffusion of the anesthetic solution through the periosteum and the minute foramina in the cortical plate to reach the nerve endings in the cancellous bone. Accordingly this technique is indicated for young and adult patients undergoing cavity preparation, root canal therapy, tooth extraction and surgery involving the alveolar bone in all the maxillary region and anterior mandibular region.
Injection Techniques
Buccal and lingual injection technique
- Preinjection preparation is carried on (see page --). The needle, a 25 gauge short needle (1 inch), is mounted in a cartilage syringe which is held in pen grip. The needle is inserted with the bevel toward the surface of the bone and the direction of the needle is at 45o angle with the buccal cortical plate. (Fig. 7-1)
- The point of needle insertion is located by the point of intersection of two imaginary lines. The first line is parallel to the long axis of the tooth to be anaesthetized and dividing it longitudinally into two equal halves and the second line is a horizontal line made by the mucobuccal fold. (Fig. 7-1 and 7-2))
- The needle is inserted through the soft tissue until the bone is reached. This is known as the needle meets resistance. The tip of the needle is now in the immediate vicinity of the periapical region of the tooth to be anaesthetized.
- The needle is held firmly in that position and about 1.5 cc of the solution is slowly deposited in the area. The needle is then withdrawn gently.
Palatal injection technique
- The point of needle insertion is located midway between the cervical margin of the tooth to be anaesthetized and the midline of the palate. (Fig. 7-3)
- The syringe is held in a pen grip and directed from the other side to be at right angle to the vault of the palate with the bevel toward the bone surface. (Fig. 7-3)
- About 0.2 to 0.3 cc of the anaesthetic solution is injected slowly in the area. This will give adequate anesthesia to the palatal mucoperiosteum in the area. It should be mentioned here that injection of a large volume of the anaesthetic solution may result in sloughing and ulceration of the palatal mucosa.
- The palatal injection should not be given more posteriorly than the level of the palatal root of the second molar otherwise anaesthesia of the lesser palatine nerve which supply the soft palate will occur. This result in dropping of the soft palate on the posterior one third of the tongue which leads to sensation of nausea and vomiting.
NERVE BLOCK INJECTIONS
In this technique of analgesia the anaesthetic solution is deposited on the vicinity of the main nerve trunk supplying the area to be anaesthetized.
THE MANDIBULAR NERVE
Injections can be used to block the following nerves:
- Inferior alveolar nerve.
- The lingual nerve.
- The mental and incisive nerves.
- The long buccal nerve.
THE MAXILLARY NERVE AND ITS BRANCHES
Injections can be used to block the following nerves:
- The posterior superior alveolar nerve.
- The middle and anterior superior alveolar nerve.
- The greater palatine nerve
- The long sphenopalatine nerves.
MANDIBULAR NERVE BLOCK INJECTION TECHNIQUES
I. INFERIOR ALVEOLAR NERVE BLOCK
The nerves anaesthetized with this technique are the inferior dental nerve and its branches peripheral to the site of injection, namely the mental and incisive nerves. This well result in a profound analgesia in the following areas:
- Body of the mandible and the inferior portion of the ramus.
- All mandibular teeth at the site of injection.
- Buccal mucoperiosteum and the underlying tissues anterior to the mandibular first molar.
Indications
- Operative and endodontic work in all mandibular teeth.
- Surgery in the mandibular teeth and its supporting structures anterior to the lower first molar.
- Surgery on the mandibular teeth and their supporting structures posterior to the second premolar when supplemented with lingual and long buccal nerve block.
Techniques for inferior alveolar nerve block
A. Standard right side injection technique
• Patient position: The patient is placed in the dental chair with the head tilted so that when the mouth is opened the mandibular occlusal plane is parallel to the floor.
• Operator position: The operator stands infront and to the right side of the patient.
• Locating the site of needle insertion
- The left index finger is placed in the mucobuccal fold opposite the premolar region. The finger is then advanced posteriorly until contact is made with the external oblique ridge and then the anterior border of the ramus.
- The finger is moved up and down, on the anterior border of the ramus, until the greatest concavity is identified. This is called the “coronoid notch”.
- The finger is then turned and moved medially. First a depression well be felt and then another ridge, the internal oblique ridge. This is the retromolar triangle which has been crossed. The tip of the index finger should now rest on the internal oblique ridge while the rest of the distal phalanx rests on the retromolar triangle and the external oblique ridge.
- The finger is then moved slightly to the buccal side taking the buccal bad of fat with it. This gives better exposure to the internal oblique ridge, pterygomandibular raphe and the pterygotemporal depression.
- The point of needle insertion is located 0.5 cm infront of the finger nail at the level of the mandibular occlusal plane.
• Insertion of the needle and injection
- The patient is asked to keep the mouth opened widely during the insertion of the needle.
- The needle is inserted from the opposite premolar region side and parallel to the mandibular occlusal plane. The needle penetrates the tissue 0.5 in front of the finger nail in the pterygomandibular depression until bone is contacted.
- When the needle contact bone, it is in the region of the pterygomandibular space. The needle is then withdrawn about 1 mm and about 1 ml of the solution is deposited slowly.
- The needle is then withdrawn half the way out and 0.3 ml of the solution is deposited. This is to anaesthetize the lingual nerve. The remaining 0.2 ml of the solution is injected buccally to anaesthetize the buccal mucoperiosteum.
- The needle is then removed.
B. Standard left side injection technique
It is exactly the same as the right side technique except for the position of the operator and the palpating hand. The following can be done:
- The operator stands to the right side and slightly toward the back of the patient. The left hand is placed around the head of the patient so that the landmarks can be palpated with the left index finger. Injection is done using the right hand.
- The operator stands to the right side and slightly infront of the patient. Palpation of the landmarks is done with the index finger of the left hand. Injection is done with the right hand which crosses the left hand infront of the patient.
- The operator stands to the right side and slightly infront of the patient. Palpation of landmark is done with the right hand and injection is done with the left hand. This technique is used when the operator can use his left hand as good as his right hand.
II. MENTAL AND INCISIVE NERVE BLOCK
Blocking the mental nerve will result in anaesthesia of the lower lip as well as the mucous membrane of the mucolabial fold anterior to the mental foramen. This is manifested by tingling and numbness sensation on the lower lip It is indicated for surgery in these areas when the inferior alveolar nerve block is not possible for some reasons.
It should be remembered that the lower central incisors and to a lesser degree the lateral incisors receive some innervation from the incisive nerve of the opposite side. Therefore anaesthesia of this teeth can not be achieved by single mental nerve block.
Technique
- The mental foramen lies at the level of and just anterior to the apex of the second premolar. The opening of the foramen is directed posteriorly The apex of the bicuspid teeth is estimated.
- The cheek is retracted, this is facilitated by asking the patient to half close his mouth, and the point of needle insertion is prepared as usual.
- The needle is then directed in a posteroanterior direction and at 45o angle to the buccal cortical plate.
- About 1.5 ml of the anaesthetic solution is deposited slowly when the needle contacts bone. The area around the foramen is then massaged gently to push the solution into the foramen.
III. LINGUAL NERVE BLOCK
The lingual nerve passes deep to the lateral pterygoid until it reaches its lower border. It then runs down and forwards to a position on the lingual aspect of the lower third molar just above the posterior end of the mylohyoid line. Then the nerve passes forward to supply the lingual mucoperiosteum and the anterior two thirds of the tongue.
Blocking the lingual nerve will result in anesthesia to the anterior two thirds of the tongue, the mucosa of the floor of the mouth and the mucoperiosteum on the lingual aspect of the mandible. This is manifested by tingling and numbness of the anterior two thirds of the tongue and painless instrumentation on the areas anaesthetized.
Technique
Technique for lingual nerve block is the same as for inferior alveolar nerve block. After the needle contacts bone it is withdrawn for 0.5 cm and the solution is deposited.
Another method to block the lingual nerve is by submucosal infiltration of 0.5 ml a few millimeters below and behind the lower third molar
IV. LONG BUCCAL (BUCCINATOR) NERVE BLOCK
This nerve is a branch of the anterior division of the mandibular nerve which passes downwards between the two heads of the lateral pterygoid to reach the anterior border of the masseter behind and at the level of the occlusal plane of the third molar. Blocking this nerve result in anaesthesia of the buccal mucosa and mucoperiosteum of the mandibular posterior teeth.
Technique
Injection is made at the point where the nerve crosses the external oblique ridge at the distobuccal aspect of the lower third molar at the level of its occlusal plane.
MAXILLARY NERVE BLOCK TECHNIQUES
I. POSTERIOR SUPERIOR ALVEOLAR NERVE BLOCK
The posterior superior alveolar nerve supply the second and third maxillary molars, the distobuccal and palatal roots of the first molar, the associated mucoperiosteum, the buccal alveolar plate of bone and the neighboring mucosa. The mesiobuccal root of the first molar is supplied with the middle superior alveolar nerve.
The nerves pass downward on the posterior aspect oft he maxilla and inter a fine foramen or foramen at the distal aspect of the maxillary tuberosity above and behind the third molar.
Technique
- The operator stands in front of the patient and to his right side. The patient is asked to half close his mouth. This is to facilitate retraction of the cheek. A syringe with long needle should always be used.
- The left forefinger is moved over the mucobuccal fold in a posterior direction from the premolar region until the zygomatic process is reached. At its posterior surface the finger will rest in a concavity in the mucobuccal fold.
- The forefinger is rotated so that the finger nail face medially. The finger is then moved to be at right angle to the maxillary occlusal and at 45o angle to the sagittal plane. (Fig. 7-6)
- The needle is now inserted in a line parallel to the finger and bisecting the fingernail.
- The needle is now inserted for about 2-2.5 cm, thus passing the curve of the posterior aspect of the maxilla and come in close vicinity to the posterior alveolar foramina. The needle should never be inserted more than 2.5 cm otherwise it may penetrate the pterygoid venous plexus with possible intravenous injection and hematoma formation.
- For the same reason aspiration should be done before injection.
II. ANTERIOR AND MIDDLE SUPERIOR ALVEOLAR NERVE BLOCK
The middle superior alveolar nerve is absent in approximately 50% of patients. However, when present, it supplies the mesiobuccal root of the first molar and both upper premolars. Together with the anterior and posterior alveolar nerves it forms the superior dental plexus.
The middle superior alveolar nerve is blocked at the same time with the anterior superior alveolar nerve when an infraorbital injection is given. The analgesic solution will diffuse along the infraorbital canal to the point where the middle superior alveolar nerve originates.
Blocking these nerves will result in analgesia of upper incisors, canines and premolars, the mesial root of the first molar and their supporting structures. Also analgesia of the upper lip, lower eye lid and portion of the nose is obtained.
Intra-Oral Technique
• Position of the patient: The patient is placed in the dental chair and positioned so that the occlusal plane of the upper teeth is at 45o angle with the floor.
• Position of the operator: For the right side injection the operator stands in front and to the right side of the patient, while to the left side injection the operator stands more to the front of the patient. The thumb of the left hand is placed over the located infraorbital foramen while the index finger is used to retract the lip
• Locating the infraorbital foramen: The patient is asked to look forward while palpating the infraorbital notch. An imaginary straight line passing through the pupil of the eye and the infraorbital notch will pass through the infraorbital foramen, the second premolar and the mental foramen. When the infraorbital notch is located the finger is moved down for about 0.5 cm while a depression will be felt. The infraorbital foramen is located in this depression.
• Insertion of the needle: A 25 gauge long needle is inserted in the mucobuccal fold in either one of two directions:
- Bicuspid direction: The needle is inserted in a line parallel to the imaginary line joining the supra- and infraorbital notches, the pupil of the eye and the long axis of the second premolar if present (Fig, 7-7 D). The needle is inserted at a distance from the labial plate of bone to pass the canine eminence. The thumb over the infraorbital foramen is used to direct the needle to the foramen. The needle should not be inserted for more than 2 cm to avoid possible penetration to the orbital cavity.
- Incisor direction: The needle is directed so that it bisects the incisor of the same side from the mesio-incisal to the disto-gingival angles. The needle penetrates the tissues 0.5 cm away from the mucobuccal fold to pass the canine eminence. The thumb of the left hand is used to guide the needle to the foramen. About 1.8 ml of the solution is deposited in the area while the thumb is in place. (Fig. 7-7 C)
Extraoral Technique
Extraoral infraorbital injection should be performed under aseptic conditions. It is indicated when there is infection in the pathway of the needle when intraoral technique is used.
- After locating the infraorbital foramen as with the intraoral technique, the skin is whipped with an antiseptic solution.
- Skin and subcutaneous tissues are infiltrated to be anaesthetized.
- The needle is then inserted and directed slightly upward and laterally to facilitate its entrance into the foramen which open downward and medially. With gentle probing motion the needle enter the foramen for a distance of about 0.5 cm and 1 ml of the solution is deposited.
III. NASOPALATINE NERVE BLOCK (INCISIVE CANAL INJECTION)
The long sphenopalatine nerve supplies the mucoperiosteum, alveolar process and gingiva of the anterior part of the palate. It reaches the palate through the incisive canal and foramen.
The opening of the incisive canal on the palate is marked by the incisive papilla in the midline of the palate and just posterior to the two central incisors.
Technique
- The papilla is extremely sensitive and injection into it would be very painful. For this reason a preparatory injection is essential. This can be done by either injecting a few drops of the analgesic solution a little to one side of the papilla or injecting it into the interseptal tissue between the two central incisors.
- The needle is then inserted slowly into the crest of the papilla, in a line parallel to the alveolar bone, and advanced into the incisive foramen for about 0.5 cm. Then 0.25 - 0.5 ml of the analgesic solution is deposited very slowly.
IV. GREATER (ANTERIOR) PALATINE NERVE BLOCK
The greater palatine nerve reaches the palate through the greater palatine foramen which is situated medial to the second or third molar. It supplies the mucoperiosteum and the alveolar process of the hard palate posterior to the canine.
Technique
- The syringe is directed from the opposite side and the needle is inserted, in a point about 1 cm away from the gingival margin in-between the upper second and third molar and a right angle to the palatal bone.
- The needle is inserted very slowly until bone is encountered and 0.25 - 0.5 ml is injected very slowly.
LOCAL ANALGESICS COMPLICATIONS
The term complication may be defined as any deviation from the normally expected pattern during or after securing local analgesia.
Classifications
Complication of local analgesia can be classified as follows:
- • Primary of secondary: Primary complication is that which is caused and manifested at time of securing the analgesia, while secondary complication is that which is manifested later though it may be caused at time of securing the analgesia.
- • Mild or sever: Mild complication is that one which exhibited slight change from the normal pattern while sever complication is that one that is manifested by sever deviation from the expected normal pattern.
- • Transient of permanent: Transient complication is that one which leaves no residual effect while permanent complication, on the other hand, leaves residual effect whatever minor it is.
Complications may be further divided into those which are attributed to the solution used and those which are attributed to the insertion of the needle. (Table 8-I)
COMPLICATIONS ATTRIBUTED TO THE SOLUTION USED
I. TOXICITY
The term toxicity or toxic over dose refer to the symptoms manifested as a result of over-dosage or excessive administration of the solution.
Etiology
The occurrence of toxicity depends on the presence of a sufficient concentration of the drug in the blood stream to adversely affect organs most sensitive to the drug which are the central nervous system, the cardiovascular system and the respiratory system. To reach a sufficient blood stream concentration the drug must be absorbed into the systemic circulation in a rate more than the rate of its biotransformation and elimination. Accordingly toxic overdose may come about by one of the following ways:
- • The use of too large volume of the solution.
- • Accidental intravascular injection.
- • The use of too great concentration.
- • Unusually rapid absorption into the blood stream as when injection is made in an extremely vascular area. Also rapid injection increases the rate of absorption of the drug.
- • Slow biotransformation of the drug as in cases of advanced liver diseases.
- • Slow elimination of the drug from the body as in cases of impaired kidney functions.
Signs and symptoms
Toxicity is usually manifested by an early central nervous system depression followed by a proportionate degree of depression. On occasion central nervous system depression may appear as the first sign. Table8-2 shows a list for signs and symptoms of stimulation and depression phases.
Prevention of toxicity
As a general rule prevention of the occurrence of complication is better than waiting until it happened and treating it. The symptoms of toxic overdose although easy to recognize and treat, it may , in some occasions occur in such rapidity that it is impossible to be treated successfully. This fact emphasizes the necessity of prevention rather than treatment. The chance for the development of systemic toxicity can be greatly decreased by applying the following rules:
1. Pre-analgesic evaluation of the patient
This is a must to detect any systemic condition that may affect the biotransformation and elimination of the drug.
2. Use the least possible volume
The belief that if a small volume is good a larger volume is better is not true. There is an optimal volume of the solution that produces satisfactory analgesia. The use of greater volume will not improve the analgesia it only increases the possibility of toxicity to occur and/or cause local tissue damage.
3. Use the weakest possible concentration
Like the volume of the analgesic solution used the use of greater concentration will not improve the analgesia. For example 1% procaine will secure adequate analgesia, 2% or 4% concentration can not do any more other than increasing the chance for development of toxicity
4. Slow injection
The solution must be deposited slowly into the tissue. Rapid injection increases the rate of absorption of the solution thus enhancing the possibility of toxic reaction. Also rapid injection may cause local tissue damage.
5. Aspirate before injection
This is especially true when injection is made in highly vascular area as when doing posterior superior alveolar nerve block. Aspiration before injection will decrease the possibility of accidental intravascular injection.
However, it must be beard in mind that failure to aspirate blood does not mean that the needle is for sure not in a blood vessel. Factors like viscosity of the blood, collapse of the wall of the blood vessel upon aspiration and occlusion of the needle by soft tissue may give a false sense of security. For these reasons, the operator should inject the solution slowly while watching the patient for any unusual reaction.
6. The use of vasoconstrictors
All local analgesic agents are vasodilators and as such they are rapidly absorbed into the circulation which increases the possibility for toxic reaction. Accordingly vasoconstrictor agent must be added to the solution unless otherwise contraindicated.
Treatment
The symptoms of toxic overdose should be recognized at the very early moment of their appearance. This means that the patient must be observed during the injection and for a considerable period of time after the injection. The sooner the symptoms are recognized and the treatment instituted the more is the chance for favorable results. Table 5-III shows an outline for the treatment of toxic overdose.
II. VASOCONSTRICTOR TOXICITY
A systemic toxic reaction is manifested when a sufficient high toxic blood level of the drug is reached. The same factors governing the rate of absorption, biotransformation and elimination of the local analgesic drug are applied for the vasoconstrictor. Signs and symptoms of vasoconstrictor toxicity include palpitation, tachycardia, hypertension and headache. Apprehension and restlessness also occur but they are very difficult to be differentiated from those due to the local analgesic agents. However, the treatment of both types of toxicity is the same.
III. ALLERGY
Drug allergy may be defined as a specific type of hypersensitivity to a chemical compound brought about by alteration in the body’s reaction to an antigenic substance. Allergy, however, is an uncommon reaction which contribute for less than 1% of the local analgesic complications.
Etiology
The primary cause of allergy is a specific antigen-antibody reaction in a patient previously sensitized to this particular drug or chemical compound. Figure 8-1 shows a schematic presentation for the mechanism of allergic reaction.
Signs and symptoms
Signs and symptoms may be mild or sever, immediate or delayed. Symptoms are exhibited by the shock organs which are the skin, mucous membrane and blood vessels. There may be:
- • Skin rashes.
- • Urticarial.
- • Angioneurotic edema.
- • Mucous membrane congestion in the form of rhinitis and asthmatic symptoms.
Delayed reaction: This may result when injection is done in patient previously sensitized. As a rule delayed reaction are more annoying than serious. Manifestation may be in the form of local edema at the site of injection, serum sickness and malaise and joint pain and tenderness.
Prevention
1. Adequate pre-analgesic evaluation: The history is the most valuable means for securing important information:
- • Patients with history of asthma and hay fever are considered potentially allergic individuals and are more liable to develop allergy.
- • When the patient gives history to a specific drug, named by the patient, he may be given another drug. But if the patient is uncertain about the name of the drug to which he is allergic, it is advisable to do allergic test for different drugs.
2. When the patient gives history of allergic reaction: No drug should be used if the patient gives history of previous allergic reaction. Also no patient should be tested to disprove his allergic history. This may result in serious complications.
Treatment
In mild cases no treatment is required but the drug should not be used in the future. In moderate and sever cases antihistaminic and epinephrine are given together with aminophylline and oxygen administration if the patient is asthmatic.
IV. ANAPHYLACTIC REACTION
It is a form of allergy that is characterized by its sudden onset during or immediately after the administration of the drug. It is one of the most urgent emergencies in the dental office.
Clinical Manifestations
There is sudden loss of the vasomotor tonus resulting in increase in the vascular bed which leads to:
- • Sever hypotension.
- • Weak pulse.
- • Unconsciousness.
- • Cyanosis.
- • Death.
Treatment
In the majority of cases death is a must unless the treatment is immediate and accurate. Treatment modalities are:
- • The patient is placed in shock position to assist adequate blood supply to the brain.
- • Respiration is immediately supported by demonstration of oxygen, artificial respiration or mouth-to-mouth breathing.
- • The circulation should be supported and the hypotension overcomed by the demonstration of intravenous fluids, vasopressor drugs and steroid hormones.
- • Closed chest cardiac massage may be needed if circulation failed to respond to previous measures.
V. IDIOSYNCRASY
The term idiosyncrasy is often assigned to a bizarre type of reaction that cannot be classified as toxic or allergic. It has been claimed that true idiosyncratic tube of reaction do not exist. The manifestations exhibited when a subtoxic dose is given represent a true toxic reaction in a patient who is sensitive to the drug.
Reactions other than toxic or allergic are usually not related to the analgesic solution. This is most probably psychogenic in nature.
VI. LOCAL REACTIONS
A. Infection
Infections due to contaminated solution are very rare at present time. This is due to the rigid standards under which the analgesic cartridges are manufactured, so that they reach the dentist as sterile ampules. However, the following should be noticed to prevent the chance of using a contaminated solution:
- • The cartridge is only used for one patient and any remaining amount is discarded.
- • The cartridge is stored dry in a sterile container that is kept covered all the time.
- • Do not store the cartridge in alcohol or any other solution. Leakage allows the alcohol or the storing solution to seep into the ampule. If an alcohol contaminated solution is injected, prolonged analgesia and local tissue irritation will result. Disinfection of the ampule is done by placing it for a limited time in a colored solution to see if leakage occurred.
- • Always handle the cartridge by the stopper end and the end containing the rubber diaphragm should be sterilized with alcohol sponge before use.
B. Local tissue damage
This may result from too rapid injection and the use of large volume especially in the confined areas as the palate.
COMPLICATIONS ATTRIBUTED TO NEEDLE INSERTION AND TECHNIQUE USED
I. SYNCOPE
Syncope or fainting is the most common complication associated with the use of local analgesia. It is a form of neurogenic shock which occurs due to cerebral ischemia secondary to vasodilatation of the peripheral circulation. This will result in sudden drop in the blood pressure. As the patient is sitting in the dental chair the brain is in superior position and is liable to reduced blood flow.
Clinical manifestations
Syncope is not always associated with loss of consciousness. Loss of consciousness is an extreme manifestation of cerebral ischemia that is sufficient to interfere with cortical function of the brain. In most cases the patients becomes pallor, dizzy and complain of feeling different or strange.
Proper management of the patient at this stage usually result in complete recovery. However, in sever case or if proper management was not taken, there may be:
- • Changes in respiratory pattern which is accompanied by extreme pallor and cyanosis.
- • Cardiac arrhythmia with weak pulse.
Treatment
Syncope is better to be managed at its early phase and before loss of consciousness. The following should be done:
- • The performed procedure is discontinued.
- • The patient is placed in semirecling position (Shock position). The back of the chair is tilted so that the head is elevated 5o and the legs are elevated 20o. This position will aids the venous return from the lower portion of the body and assist adequate blood supply to the brain.
- • If the patient is conscious he is instructed to take few deep breaths. This will assist the venous return and provide adequate oxygenation.
This simple management is usually enough and the patient regains his normal feeling. The patient should now be reassured and reevaluated. However when the more sever symptoms of cyanosis and cardiac arrhythmia are present the respiratory and circulatory supportive measures should be taken.
II. MUSCLE TRISMUS
Trismus (inability to open the mouth normally) is a common complication particularly after inferior dental nerve block.
Etiology
- • The most common cause is trauma to the muscle during needle insertion.
- • Injection of an irritating solution.
- • Hematoma formation in the muscle.
- • Low grade infection within the muscle.
Prevention
- • Use sharp sterile needle.
- • Insertion should be as atraumatic as possible.
- • The area of needle insertion should be cleaned and painted with nonirritant antiseptic solution.
- • Avoid repeated injections.
Treatment
In most cases no treatment is necessary and the condition corrects itself. However, when it is due to muscle trauma muscle exercises and analgesics may be needed. When hematoma formation or low grade infection is expected mouthwashes and antibiotics may be required.
III. PAIN
Pain during or after injection is very common and in most cases it is due to carelessness on the part of the operator.
Prevention
- • Always use sharp needles.
- • Area of penetration should be painted with topical analgesic.
- • Insertion should be made as atraumatic as possible.
- • Multiple insertions in the same area should be avoided.
- • Injection should be injected slowly.
- • Injection of large volume in constricted areas, as the palate, should be avoided.
- • The solution temperature should be as close to the body temperature as possible. Too hot solution is more harmful than too cold solution. This is achieved by holding the analgesic cartridge in hand of the operator for few minutes before injection.
IV. EDEMA
Edema is rather a symptom and not an entity in itself. Trauma, infection, hemorrhage allergy can produce edema. Treatment depends on the cause.
V. INFECTION
Infection may result from the use of nostril needles or solution or from carrying surface bacteria from non-sterile mucosa into the deeper tissue by the tip of the needle.
VI. PROLONGED ANALGESIA
Prolonged analgesia may occur due to the following causes:
- • Prolonged analgesia may occur due to injection of a solution contaminated with alcohol or other sterilizing solution.
- • More commonly this complication is due to trauma to the nerve sheath caused by the needle which results in hemorrhage into the nerve sheath. In such cases the patient will report an electric shock in the areas innervated by the traumatized nerve. The resultant hemorrhage undergoes resorption very slowly due to the poor circulation of the area.
- • Trauma and swelling of the soft tissue in the proximity of the nerve.
Treatment
In almost all cases of prolonged analgesia the condition returns to normal with treatment.
VII. HEMATOMA AND ECCHYMOSIS
Hematoma is the diffusion of blood into the tissue as a result of punctured vessel. It is usually associated with infraorbital nerve block and posterior superior alveolar nerve block. All hematomas are absorbed in due time with no residual effect other than the skin discoloration which may persist for few days. No attempt should be made to aspirate or to otherwise interfere with the normal absorption of the blood as the condition has no complications.
VIII. BIZARRE NEUROLOGICAL SYMPTOMS
On rare occasions unexplained neurological manifestations may occur during or after administration of local analgesia. These may be in the form of facial paralysis, crossed eyes, temporary blindness ...etc.
Occurrence of such symptoms is quite rare. However, the best method of prevention is to follow closely the accepted techniques and to adhere to all basic concepts of accepted procedures.
IX. LOCAL TISSUE DAMAGE
Sloughing and ulceration may occur if the analgesic solution is too rapidly injected in the tissue or too much volume is used. This is especially true in confined areas as the palate and the labial aspect of the lower teeth.
X. BROKEN NEEDLE
This complication is one of the most annoying and depressing complications. This complication is quite uncommon at present time due to the use of single-used needles. However, for this complication to occur it needs a great deal of carelessness on the part of the operator.
Prevention
- • Never force the needle against resistance. Needles were never made to be forced into bone or beneath the periosteum.
- • Never change the direction of the needle inside the tissue. Always withdraw the needle to just below the mucosa and redirect it.
- • Do not use needles with too fine gauge.
- • Do not use resterializable needles. Resterialization of the needle makes it dull and more liable for breakage.
- • Never insert the whole needle inside the tissue. As a rule 1/3 of the needle must be in view outside the tissue so that if breakage occurs, usually at the hub, the needle can be removed by grasping the portion in view outside the tissue.